PERIODONTAL DISEASE – BACTERIAL INFECTION.
95% of the more than 700 species of microorganisms residing in the oral cavity are represented by harmless helpful bacteria classified as gram positive aerobic (oxygen loving) strains. Only less than 5% will be associated with periodontal disease and they are mostly represented by gram negative anaerobic strains of bacteria (anaerobic: keeping away from oxygen). Inflammatory disease cannot develop without these bacteria. The most implicated bacteria in chronic periodontal disease characterized by deep periodontal pockets and high resistance to conventional treatments are: Actinobacilus, Actinomycetemcomitans, Porphyromonas Gingivalis, Tannerella Forsythia, Treponema Denticola, Treponema Socranskii, and Porphyromonas Inermedia.
P. Gingivalis produces enzyme arginine-specific cysteine proteinase which disrupts the immune system and leads to periodontal connective tissue destruction. The bacterial trio T. Denticola, P. Gingivalis, B. Forsythos also known as “RBC” red bacterial complex, associated with most severe forms of periodontal disease possese enzymes capable of hydrolyzing the synthetic peptide benzoyl-DL-arginine naphthylamide (BANA).
Treponema Denticola, Porphyromonas Gingivalis, Tonnerella Forsythia previously known as B. Forsythia.
(RBC) ” The red bacterial complex ” always present in severe periodontal disease, its presents can by detected in samples taken from periodontal sulcus through enzymatic test resolts avilable after seven minutes of incubation.
Based on this unusual enzyme Dr. Walter Loesche and colleagues at the University of Michigan School of Dentistry developed a highly sensitive test specific to this bacteria which allows early detection and diagnosis of periodontal disease. In view of the overwhelming evidence supported by research, accepting the existing paradigm that periodontal disease is limited to gums, alveolar bone and teeth is no longer possible. We have to accept the truth and face the fact by redefining the existing definition of the disease to the new paradigm that periodontal disease is a systemic contagious condition, by nature inflammatory to the whole body, in which all the life sustaining organs are under direct threat. Early diagnosis, antimicrobial therapy, microscopic monitoring of treatment, efficacy and intervention in transmission of pathogenic bacteria must become the standard of care in control of caries and periodontal disease, followed by systemic intervention to eliminate the pathogen from the body. In order to fulfill this promise it will be essential to scrutinize prevailing methods, protocols, applied standards and recommendations offered by the dental profession. The scrutiny will be narrowed to the field of periodontal disease.
Reflecting on all the information presented and the assessment of current standards and rationales based on outdated research, it will be appropriate to revisit them and expose the inadequacy of offered procedures currently widely used for treatment of periodontal disease. In order to attempt this evaluation it will be necessary to bring forward the newest research to date available to gain understanding of the processes taking place in the human mouth and how they are affecting the dynamics of the disease.
Mitochondria are the cell's power producers. They convert energy into forms that are usable by the cell.
The bacterial diversity in human oral cavity is estimated to be more than 700 different species and phylotypes, belonging to nine phyla: Defembacteres, Spirochaetes, Fusobacteria, Actinobacteria, Firmicutes, Bacteroidetes, Proteobacteria and newly discovered none cultivable two phyla members OP11 and TM7. We have to acknowledge that bacteria are essential to our existence in this earthly environment and are playing a leading role in many life sustaining processes. For example, mitochondria were once living prokaryotes (cells that lack nucleus and organelles) and took up residence in large cells and developed a relationship that is so successful that now the cell would die without them. They are in every cell of the human body, except red blood cells. They have their own DNA and multiply separately from cell division. Mitochondria are responsible for 90% of the chemical energy production for the cell. Chloroplasts have a similar function in the cells of plants.
The three pounds of bacteria in the human digestive tract are working to break down our food, to realize nutrients which will be absorbed by the body. 95% of the bacteria are helpful in commensal relationship with the host. The remaining 5% are potentially pathogenic and only a few will be strictly pathogenic with parasitic characteristics.
They are the ones capable of polymorphic metamorphosis, adapting to the form most suitable to survive in newly acquired environments; they are the ones which provoke the organism to acute inflammatory response and which paradoxically will aid them to break entry from the inflamed gums to the bloodstream and from there to every organ of the body. They hide in the bio-film of sub-gingival calculus with extra protection by meniscus of cervicular tissue fluid from antibiotics and chemicals of mouth rinses.
Next time when you take a mouth-rinse which kills 99% of germs, think for a moment: what germs? I have never seen anybody who has slowed down the periodontal disease with mouth-rinses but I have seen many who developed candidacies (fungal infection of the mouth) which will easily turn systemic.
The mouth is a very valuable piece of real-estate when you wipe out the occupants, meaning your good bacterial flora. The fungus will take over or other parasitic strains of bacteria, but your infectious bio-film bacteria occupying gummy sulcus around your teeth will survive unaffected.
It definitely looks like we have problem and a dilemma when dealing with this situation. Our concern will make us seek professional help from the dental office. The most commonly prescribed procedure will be teeth cleaning, also known as prophylaxis. The procedure is performed by a dentist or dental hygienist with a rotary instrument equipped with prophy cup filed with abrasive paste usually (pumex based). When properly administrated, it will remove most of supraginival plaque and some subgingival, providing that the plaque is not mineralized. This procedure is recommended as a follow up after a more invasive procedure of deep cleaning, also known as scaling and root planing.
Standard recommendation is to come every 3 months, provided that you will perform meticulous and judicious oral hygiene regime of brushing and flossing after every meal. The recommendation is based on an obsolete study that determined that it takes 90 days for plaque to mature and if a dentist intervenes again in that period of time this will control periodontal disease.
The newer, more sophisticated research has determined that immediately after creating a clean surface of the tooth, in the next 30 seconds that surface will be coated with salivary mucosal protective film called pellicle. The film’s physical properties, such as viscosity and strength, are the result of complex interactions between different proteins within the saliva and other components such as calcium and other salts, food proteins and emulsifiers. Immediately afterwards, the gold rush begins: all the bacteria from the vicinity and saliva will start the colonization of available surfaces and bio-film formation. Providing that one cubic millimeter of saliva approximately contains 10 to 9th power of bacteria we are starting the process with astronomical numbers of colonizers.
The average amount of time required for the division of the bacteria in a colony is 15 minutes, and the numbers double and so in the next 15 minutes double again and again providing that the substrate (food) is available. In 8 hours, after a professionally executed procedure, we have a completely brand new bio-film ecosystem established, and all destructive processes of resorption and chronic inflammatory processes are engaged in the dismounting of our periodontium.
The therapeutic value of this procedure is less than 8 hours. If someone wanted to be sarcastic, the new recommendation would be to come to the dentist every 8 hours. Totally impractical.
It would be interesting to know how much substrate (food) is needed to fully saturate the metabolic rate of all the bacteria in oral flora. The answer comes from a 25 year old French study. After the preparation of teeth with prophylaxis and polishing and rinsing with water, the base for the study was established. Then one drop of orange juice was placed on the tip of the tongue and the measurements were performed. For 7 minutes the graph almost vertically climbed up then reached a plateau, bacteria were saturated and adding more substrate would not change the rate of metabolism, (metabolic rate in this context means division of bacteria every 15 minutes). The plateau of full saturation lasted for 3 hours and in 45 minutes, then dropped down to the baseline.
This information is eye opening. The amount of food needed to saturate the bacteria’s metabolic rate in the mouth for 3 hours and 45 minutes is infinitely small compared to the amount of food in our meals and the frequency of them correlates with the interval of saturation, not to mention the snacks between the meals.
The scaling and root planing or deep cleaning is a very invasive procedure especially when it is performed under local anesthesia which contains adrenaline. The medication is a very strong vasoconstrictor, responsible for shutting off blood circulation in the area of micro surgery and practically paralyzing the immune defenses for the period of the procedure, when the instrumentation and manipulation of the tissues stirs up the bacteria and causes massive bacteremia in the blood of the patient.
Anesthetic procedures and surgery increase the occurrence of bacteremias up to 97%. Dissemination of oral microorganisms into the bloodstream is common and in less than one minute after the oral procedure, organisms from the infected site may have reached the heart, lungs and peripheral blood capillary system (Clinical Microbiology Review Oct. 2000). There are some horror stories of complications after these procedures, and in some cases there has been a need for hospitalization of the patients. Scaling and root planing is expensive, labor intensive, and time consuming, and lethally delegated to the dental hygienist by most dentists. Based on recent findings the therapeutic value of this procedure lasts for 8 days.
Gum surgery, the most invasive and most expensive procedure, the bread and butter of periodontists, has similar therapeutic value to deep cleaning. Dr. Arthur Merritt, a highly respected New York periodontist and a president of ADA (American Dental Association) stated “Surgical periodontia is an indictment of the dental profession made necessary only because of its failure to live up to its responsibilities in the prevention and early treatment of periodontal disease.” And nothing can be truer than this statement. Dr. Paul H. Keyes the founder and developer of “Keyes method” of non-surgical control of periodontal disease noted: “ If you are going to scrape around the teeth, you’re not more than the janitor going around cleaning up the office – janitorial services…a janitor of the mouth.” Dr. Keyes had this to say about gum surgery: “ Unnecessary disfigurement of the mouth.”
To me, gum surgery is a hopeless chase after despairing alveolar bone which leaves the patient with horsey looking teeth. It will not stop bone resorption nor the disease. The rationale for this surgery is to reduce pocket depth as close as possible to physiological levels. Patients who choose this treatment modality usually will have multiple surgeries through their lifetime.
The three basic methods presented above used in dental offices to control periodontal disease and home care instruction of brush and floss have one thing in common: they are all mechanical in nature and the only thing you can achieve by using them against a living biological environment is to disorganize and disperse, nothing more. And now we know for how long (8 hours to 8 days ). It will not eliminate bacteria nor neutralize any by-product or toxins they produce.
It is similar to finding an ants’ nest and stirring it up with a stake. In a very short time, the nest will be reconstructed and in full operation. It will be interesting to visualize the scale of these mechanical devices in relation to the bacteria they are intended to be used against. On the tip of one bristle of your toothbrush you can place hundreds of thousands of bacteria. The dental curette use by the dentist to scrape your teeth, compared to a single bacteria will be as big as New York’s tallest skyscraper. You can imagine the precision these devices can achieve in this micro world. It is almost the same as if you have an expensive Swiss watch and somebody gives you a hammer and sickle to repair it. And yet the majority of dentists using this method routinely will claim the success of relieving their patients from suffering with good results, the modality of which will be substantiated as a valid and helpful treatment by scientific study.
But that will be only true if we measure the success on the basis of remission of symptoms. Statistically, the majority of patients will look for professional help when the periodontal disease turns from the chronic symptomless state of inflammation, to the very painful acute state of inflammation. The body responds in very rewarding ways to these treatments, leaving the professional with satisfaction and the patient relieved with a feeling of gratitude, believing that everything will be fine. What happens here is that it is relatively easy in early state of the disease to bring the body to the state of equilibrium between the pathogen virulence and host defenses, back to the original state of chronic inflammation.
However, there was no cure here because the cure was never attempted. The pathogens were never identified, nor considered as probable cause for this condition. This situation will repeat itself again and again then with higher frequency and finally the patient will be in state of “chronic acute infection” a state of pyorrhea with pockets up to 9-10 mm. There will be no treatment for this condition except for tooth extractions, as there will be no more alveolar bone left.
But from the perspective of the periodontist this is a new opportunity for windfall profits. Yes, these patients are candidates for dental implants. This time a full mouth restoration will be equivalent to the price of a new Mercedes and ironically the post operative instruction to the patient will the familiar, brush and floss your implants.
The logic of this is overwhelming, how is it possible that this mechanic who failed to save your teeth, this time will save your implants? Dental implants are more susceptible to bacterial infections than natural teeth, and the failure of an implant has much more serious consequences than the loss of the tooth. The time for treatment and the opportunity to address the true cause of the disease was wasted in those 40 years of pursuing the symptoms, never attempting the cure. The only thing which allows this status quo to exist is that the disease itself takes 40 to 50 years to claim the teeth. But at this time it is actually claiming the whole body.
In order to have an understanding of periodontal disease we have to gain the understanding of two underlying processes that are associated with this inflammatory condition. One is alveolar bone resorption and the second is penetration of the bacteria through inflamed gums into the blood circulation. We know that bacteria cannot resorpt the alveolar bone or any bone. If that were to be the case, we would never have found 60 million year old fossilized skeletons of dinosaurs, or other animals or humans. To resorpt the bone you have to have specialized cells that are equipped with a battery of enzymes and chemicals suitable for the task.
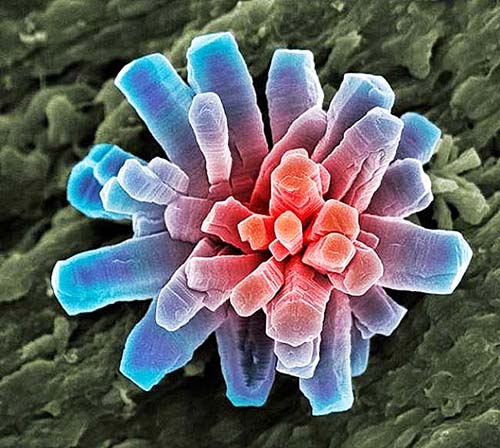
The cells capable of these assignments are the osteoclasts (bone resorpting). They are a specialized macrophage polykaryons whose differentiation is regulated by a colony stimulating factor RANK ligant and osteoprotegrin and osteoblasts (new bone forming large cells, originating in bone marrow). Without these cells in our body, our broken bones would never heal. The exact processes of initiation of bone resorption are not clearly understood but there is enough data available to have a general understanding of the phenomena. To initiate the process of bone resorption there has to be an accumulation of osteoclasts in the area, the stimulating factors responsible for osteoclasts’ differentiation, RANK and osteoprotegrin, have to be activated. The pathological strains of bacteria like Porhyromanas Gingivalis, Campylobacter Rectus, Acinobacilus Actinomycetemcomitans, and Fusobacterium Nucleatum are known to induce in the host cells several factors, such as lipopolysacharides (LPS), interlukin-1 (IL-1) and (IL-6), tumor necroting factor (TNF), vesicles toxins and enzymes. (Infected Immune Sept. 1998). Some of these factors like inerlukin-1 (IL-1) are considered as the marker of osteoclastic activity and when combined with specific fluorophores will be visible under a fluorescence microscope (which gives the opportunity for quick chair-side diagnosis).
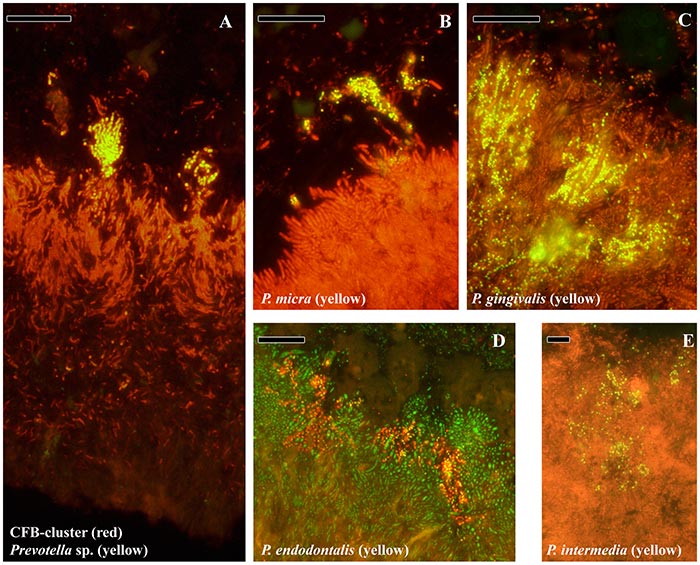
Localization of species of bacteria associated with periodontitis in bio-film matrix.
Photo: Overview of the subgingival biofilm with CFB-cluster species (red) and Prevotella sp. (yellow). Since Prevotella sp. are part of the CFB-cluster of bacteria, cells appear in yellow. (B) Top of the biofilm with a micro-colony of P. micra (yellow). (C) Micro-colonies of P. gingivalis (yellow) in the top layer. (D) Micro-colonies of P. endodontalis (yellow) in the top layer. (E) Micro-colonies of P. intermedia in the top layer. ( Courtesy of Vincent Zijnge, M. Barbara M. van Leeuwen, John E. Degener, Frank Abbas, Thomas Thurnheer,Rudolf Gmür,Hermie J. M. Harmsen )
The group of bacteria associated with periodontal disease when organized into bio-film matrix is capable of producing sophisticated chemicals that allow them to modulate the surrounding environment. They all are anaerobes and by inducing osteoclastic activity (bone resorption) they achieve substantial improvements of their anaerobic ecosystem. Deeper pockets offers more protection, less oxygen, and when combined with matrix formation and allowing other bacterium to join the bio-film home, the community is capable of full control of the activities in periodontal pockets. The bio-film strength comes from the diversity of bacteria and combined gene pool at its disposal. Everybody is working for benefit of all, an “E Pluribus Unum” at its best.
The pocket is converted to a well organized base which will be used as the launching port for the assault on the border. The ultimate goal of this pathogenic bacterium is to break entry into the host circulatory system and then fully exploit its parasitic capability (polymorphic, many-forms, changing forms, intracellular and extracellular, “Russell Bodies,” nanobacteria).
ACUTE INFLAMATORY RESPONSE
When everything is prepared in the environment of a chronic state of equilibrium between pathogen virulence and host defenses, the bio-film community through quorum sensing and quorum acting will induce from the host the acute inflammatory response characterized by five classic signs of inflammation: Rubor (redness) increased vascularity, Tumor (swelling) exudation of serum fluid, Calor (heat) increased blood flow and inflammatory mediators, Dolor (pain) stretching of pain receptors and nerves by inflammatory exudates and chemical mediators, Funcio Lesa (loss of function).
One of these five classic signs of acute inflammatory response will directly aid the bacteria for its entry of pathogen or fragments of bio-film in to the capillary vessel. That sign is Tumor (swelling). When bacteria or their toxins are recognized by the immune complement system, it in turn produces chemical messengers ( cytokines ) which will warn other cells of the immune system that the body been invaded. There will be general mobilization, known as immune-cascade, and an urgent need to create extra space to accommodate this massive concentration of large immune cells and proteins into the area of inflammation. The chemical mediators are released from plasma cells, including mast cells, platelets, neutrophiles and monocytes/macrophages like histamine and other vasodilators. They are injected into the bloodstream, causing dilatation of the blood vessels which in turn increases permeability of the capillaries and separation between endothelial cells, allowing for a massive exodus of serum exudates into extracellular space and migration of phagocytes outside the blood vessels.
This condition will be visible as a swelling capable of enlarging the area up to five times compared to the healthy state. Macrophages begin life as monocytes which originate in the stem cells of the bone-marrow, but when they are called to action they turn to macrophages. There are stationed in strategic locations through the body and are the front line defense against bacteria invasion.
This rapidly created aquatic open highway allows for navigation and piloting of macrophages and leukocytes to the areas of concentrated bacteria invaders. The piloting is literally the same as the transport of heavy equipment on the freeway: the small mobile pilot car in the front, and one behind the machine. The classic military strategy is applied: circumscribe, isolate and destroy. So an acute infection will be eliminated and we will recover and get back to normal, quickly forgetting the incident.
But that will not happen in the case of gum inflammation infected with these known pathogens. The acute inflammation will be brought back to its chronic state of equilibrium between pathogen virulence and host defenses and the process will go on and repeat itself again. But an open highway is a two way street; if something gets out something always will get in. This changed environment creates an opportunity for motile bacteria to break entry, and by simply positioning themselves near the emerging macrophages they will be sucked in by the closing capillary wall.
What happens later we already know. After the battle is over, most cells participating in the event will die and the proteins, dead bacteria and chemical debris will be organized to pus and extracted from the body. The cells in the body after exhausting their life cycle in normal circumstances will die by “committing suicide” (apoptosis-death of cells in normal fashion).
CHRONIC INFLAMMATION, BIOFILM, CALCULUS FORMATION
However in cases of chronic inflammations, the situation is different. Helper T-cells emit a “stay alive” signal, and keep emitting the signal as long as they detect a foreign antigen in the body. This allows the cells that have exhausted their life cycle and accumulated irreversible damage to stay alive and divide, producing compromised sister cells which eventually will turn carcinogenic.
This is the mechanism by which prolonged (chronic) infections become the cause for cancer formation. To simplify the matter and summarize: the nature of periodontal disease lies in the capability of specific strains of bacteria to send signals through messenger proteins to activate osteoclastic activity and they will maintain this status as long as the pathogen is allowed to occupy the invaded site. Any mechanical manipulation alone performed by dentist or patient in its principle are subject to failure since they cannot affect or disrupt living biological processes. But they can be very helpful in aiding the pathogen to achieve its second objective: the systemic colonization of the host.
In order to make any progress with correct diagnosis (without diagnosis there is no treatment) we have to separate two distinguished processes, calculus formation and bio-film formation. Both processes are occurring independently from each other and are based on totally different principles.
First of all the calculus formation does not require presence of bacteria to form. This is a proven fact by numerous studies on germ-free laboratory animals where calculus formation was observed. The only difference was that the process of formation was slower than when bacteria was present. Calculus formation a is natural process. It is happening all over the world whenever water with dissolved calcium phosphate salts is present, not excluding saliva. Examples of this process surround us everywhere: shower heads, faucets, plumbing pipes, washing machines and nature’s magnificent stalactite formation. The following minerals are found in calculus: Brushite, octacalcium phosphate, magnesium whitlockite, an unusual form of calcium phosphate and hydroxyapatite.
When one cleans the surface of the tooth, 30 seconds later pellicle formation is completed, the bio-film formation colonizes in approximately two hours and completes the first layer of bacteria. The electrical charge of the tooth will be changed from positive to negative which will actively initiate precipitation of positively charged ions of minerals dissolved in saliva to the newly formed bacterial plaque. This process speeds the calculus formation because of active transport of ions, similar to plating baths of metals.
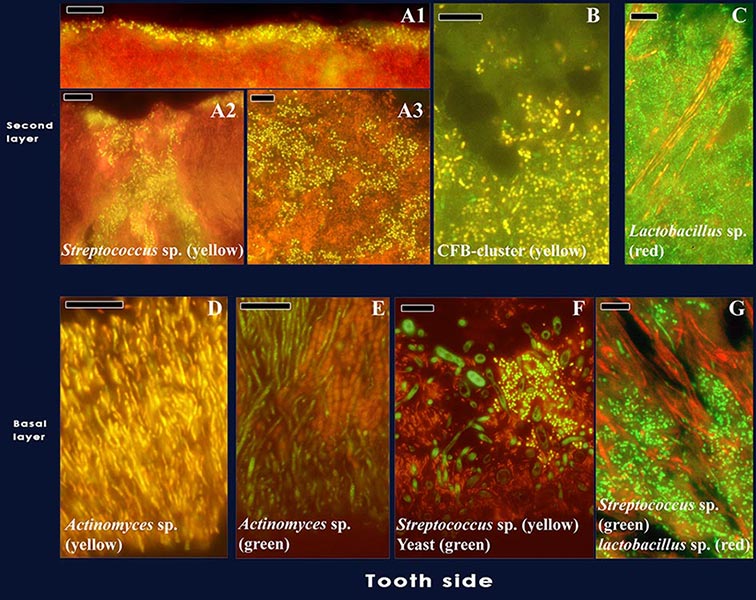
Localization of the most abundant species of bacteria in supragingival bio-films.
Photo: Localization of the most abundant species in supragingival biofilms. Streptococcus sp. (yellow) form a thin band on top of the biofilm (A1), almost engulfing in the biofilm (A2) or present as small cells scattered through the top layer of the biofilm (A3). (B) Cells from the CFB-cluster of bacteria in the top layer of the biofilm, without defined structure. (C) Lactobacillus sp. (red) forming long strings through the top layer. (D) Actinomyces sp. (yellow) plaque attached to the tooth. (E) Actinomyces sp. (green) and cocci forming initial plaque.(F) Multispecies initial plaque composed of Streptococcus sp. (yellow), yeast cells (green) and bacteria unidentified (red). (G) Streptococcus sp. (green) and Lactobacillus sp. (red) forming initial plaque. Black holes might be channels through the biofilm. ( Courtesy of Vincent Zijnge, M. Barbara M. van Leeuwen, John E. Degener, Frank Abbas, Thomas Thurnheer,Rudolf Gmür,Hermie J. M. Harmsen )
It has to be noted that saliva is exclusively responsible for supragingival calculus formation. Because both processes, bio-film and calculus formation, occur in the same environment simultaneously and physically occupying the same space, there will be competition between plaster (calculus formation) and bio-film groups which in final outcome give us the layers of a cake with always fresh bio-film on the surface.
The dynamic of bio-film formation is same in every patient providing that nutrients are available, but calculus formation differs between individuals. Some patients generate large amounts of calculus in a very short time, and some don’t have any. And of course there is going be a wide spectrum of variation between those two extremes. The subgingival calculus is derived from the gingival cervicular fluid (GCF), which is characterized by a higher potassium concentrate than serum or saliva. The results of (Sakson 161) work may indicate that the pellicle formed from GCF is colonized much faster than formed from saliva. Careful consideration shall be applied to the role GCF is playing in both health and disease. In health the GCF pH should be the same as the blood serum. It is also providing the nutrients to the cells of junctional epithelium and therefore will be the source of nutrients for the sulcus and bacteria as well.
It was observed that there is an outward flow of GCF accompanied by flushes every 40 seconds which remove bacteria and metabolic products and preventive inflow of saliva. The periodontal sulcus is a self-sustaining enclave of an ecosystem, not requiring nutrients from outside sources like the oral cavity. In disease, the composition and pH will change reflecting on the presence of inflammatory components. (Seymour 1974). The perpetual flow of GCF is reflected in matrices’ architecture of subgingival bio-film. It is like Venice, Italy built on canals up to 18 stories in height, where the nutrients from canals through capillarity are delivered to upper levels. It is an ecological marvel, utilizing all available resources of the terrain.
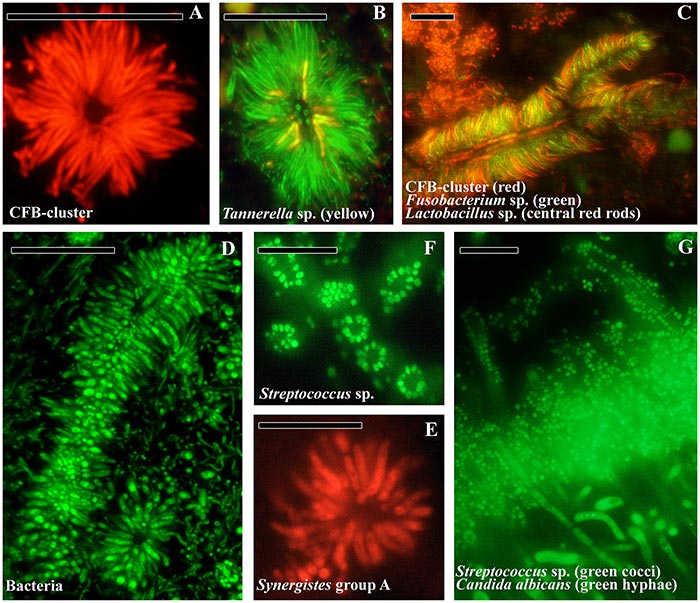
Subgingival plaque structure.
Photo: (A) Transversal view of a test-tube brush found in subgingival plaque composed of filamentous cells from the CFB-cluster. (B) Tannerella sp. (yellow) in a test-tube brush. (C) Longitudinal view of a test-tube brush with Lactobacillus sp. (red rods) as central structures. F. nucleatum (green) and CFB-cluster filaments radiating from the central structures. (D) Longitudinal and transversal view of a test-tube brush stained with the eubacterial probe. (E) Transversal view of the test-tube brush in panel D, composed of Synergistetes group A species. (F) Transversal view of Streptococcus sp. (green) aggregation around a central cell (not stained) in supragingival plaque. (G) Transversal view of supragingival plaque with Streptococcus sp. (green cocci) and Candida albicans (green hyphae) in the top layer of the biofilm and forming corn cob structures growing outwards. Bars are 10 µm. ( Courtesy of Vincent Zijnge, M. Barbara M. van Leeuwen, John E. Degener, Frank Abbas, Thomas Thurnheer,Rudolf Gmür,Hermie J. M. Harmsen ).
In my observation, I found a correlation between the pH of saliva and the amount and speed of calculus formation (we routinely measure pH of saliva in our patients). These findings are collaborated by numerous studies. The Henderson-Hasselbalch equation correlates that the increase in pH favors the formation of calculus. It appears that patients with pH 7 or more, like 7.4, will be the ones with most calculus on their teeth.
A few words about pH. 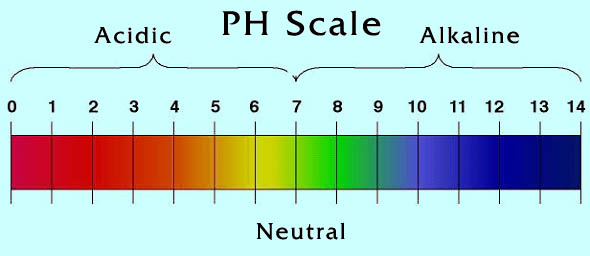
The scale of pH goes from 0-7-14, where 0 represents strong acid, 7 neutral, and 14 strong base. The scale is logarithmic which means that each step is 10 times the previous one, for example a pH 4.5 is 10 times more acid than 5.5, 100 times more acid than 6.5 and 1,000 times more than 7.5.
To grasp the concept of pH lets look at the water molecule H2O. The H20 will ionize to Hydrogen (H+) and hydroxyl (OH-) ions. When ion balance is in equilibrium the pH is neutral (7), when there are more (H+) ions than (OH-) ions then the water will be acidic, when (OH-) ions outnumber the (H+) ions the water is alkaline. Minerals with negative (-) electric charge are attracted to Hydrogen (H+) ions and they are called acid minerals like: Chlorine (CL-), Sulfur (S-), Phosphorus (P-) and they form Hydrochloric acid (HCL), Sulfuric acid (H2SO4) and Phosphoric acid (H3PO4). Minerals with positive (+) electric charge will be attracted to negatively charged Hydroxyl (OH-) ion, (this reaction is responsible for calculus formation in the presence of bio-film bacteria). They are called alkaline minerals like: Calcium (Ca+), Potassium (K+), Magnesium (Mg+) and Sodium (Na+).
calcium phosphate
The bone and teeth enamel are made out of calcium phosphate. If you have lots of positively charged Hydrogen (H+) ions in your acidic saliva it will pull negatively charged Phosphate (P-) ions right out of the tooth enamel which is known as demineralization of enamel which will lead to cavity formation. Alkaline saliva is necessary to preserve and rebuilt tooth enamel. From all these findings it is quite obvious that detection in the human mouth of calculus, bio-film or lack of calculus cannot be considered as indicators for presence or absence of periodontal disease.
While researching the subject of periodontal disease, I had an encounter with a very interesting patient. She was a 38 old female visiting Los Angeles from out of state; she insisted on having a teeth cleaning appointment on the specific date. Later on, I found out the true reason for that requirement. That day I cleaned the cleanest teeth in my life, I found out that day was a day exactly three months from her last teeth cleaning. She was the patient who followed up the dentist’s recommendation to the last detail. She showed me a toothpaste and dental floss and stated that she is flossing and brushing her teeth after every meal, she drinks only water, and does not eat between meals: a 100% compliance to standard dental recommendation.
Her gums looked healthy and pink, and I could not visually detect the slightest form of acute inflammation. “Some of most severe cases of gum disease have excellent oral hygiene.” (Dr. Keyes). The probing revealed something which I had not anticipated in her posterior region of upper and lower molars and premolars. The pockets measured consistent 6mm, in some areas reaching 7mm deep. This example illustrates and supports the fact that mechanical means alone will never control or stop the periodontal disease, and even the most meticulous elimination of food particles will have no effect on dissolved sugars in the saliva, and cervicular fluids. Remember the French study: one drop of orange juice on the tip of the tongue.
Carlson and Ryan (25) found that hyperglycemia was invariably followed by great increase of glucose in stimulated saliva. Luisda (67) established that in healthy people there is proportional relationship between saliva sugar and blood sugar. Therefore it can be stated that saliva contains glucose under normal conditions which are proportionally reflecting the level of glucose in the blood.
Based on these findings, the only diagnosis which would reflect the existing condition of this patient will be a form of advanced periodontal disease. She was in a state of shock and disbelief: “For last twenty years I never missed any of my three month scheduled cleaning appointments. Why didn’t anyone tell me this before?” And I know that she is not the only patient who has asked this question or will ask it in the near future.
This question is like echo banging in my head: “Why did not anybody tell me this before?” Can I attempt to answer this question honestly and truthfully without rocking the dental boat? The first thing will be to look at the facts: Dentistry in general is composed from three basic components, education; dental board exams; and dental practice. The fourth component which affects dental practice is industry and the fifth one is attorneys.
When in 1984 I was taking the California State Board exam, for the first time in California the Board introduced a new requirement on their practical exams for testing applicants on the proficiency of removal of sub-gingival calculus from patients. The requirement was to bring in a patient with sub-gingival calculus visible on dental X-rays. The procedure was to remove all the deposits and plane the root surface so the dental probe in the hand of dental examiner will freely glide over the prepared surfaces. If you were able achieve this goal and didn’t butcher the patient’s gums in the process, you would get passing grade and become a provider of periodontal services. There were no attempts made to recognize that this is a bacterial infection and needed to be followed with adjunctive therapy such as local delivery of antimicrobial agents or host modulation that will require monitoring of the efficacy of prescribed modalities. The truth was that in this period mainstream dentistry had nothing to offer with the exception of a few pioneering dentists who understood the underlying causes of disease and addressed the bacterial infection as the major source of the periodontal disease. Rather it was considered as mineralized deposits capable of tissue irritation and when properly removed will reverse the gums to normal state. This was based on shallow observation of the obvious. The deposits were detectable, visible and removable and everything could be resolved in macro scale so you may say what the Board requires the school will teach and the dental office will practice.
You still can find dentists today who will tell you that periodontal disease is not infectious and bacteria have not much to do with it. The first answer to the question “Why did not anyone tell me this before?” came from attorneys; they managed to successfully win big rewards in several cases by asking this question. The dental profession was caught off guard. The insurance companies quickly mobilized and started offering free of charge “Risk Management Courses” for the dentist, giving incentives in the form of continuing education credits and fee reduction for dental malpractice insurance for those who attended the seminars.
This was a smart move by the insurance companies. In a very short time this mobilized the profession and stopped the wave of malpractice suits based on periodontal disease. Interestingly there were no attempts to scrutinize or reevaluate existing procedures but instead all emphasis was directed toward diagnosis and record keeping. I do not need more evidence to convince myself and perhaps some of you who read this essay that most if not all of the human conditions we suffer from originate from the disruption of balance of microbiota in the human ecosystem, and our actions to try and restore the balance by means of overuse broad-spectrum antibiotics can further disrupt the body’s normal ecology, rendering the human more susceptible to bacterial, yeast and parasitic infections.
The most common shot-gun approaches with antibiotics and conventional mouthwashes, indiscriminately kill both benign and harmful pathogenic organisms and only for very short time (12 hours) actively disrupting the balance of microbiota.

LAKE:
Lakes symbolized aspect of feminine archetype; holds the significance of mirror; image of self-contemplation; reflection on life; escape from reality; first mirror to the man to see his reflection; fluid mass of transparency.
